Center of Imaging Sciences and Medical Physics, University of São Paulo (USP)-Brazil.
IntroductioN
Creutzfeldt-Jacob disease is a rare dementing illness caused by an agent called a prion. This entity is classified into four
main subtypes: familial forms (fCJD), sporadic forms (sCJD), iatrogenic forms (iCJD) from cadaveric hormones-related transmission
or neurosurgical procedures, and the recently described variant form (vCJD) from animal contaminated food products (1).
Approximately 90% of the cases are sporadic, without any detectable cause (1).
Probable clinical diagnosis is suggested by rapidly progressive dementia, myoclonic jerks and periodic sharp-wave electroencephalographic (EEG) activity. But the classical symptoms may be lacking in as many as 25% of the patients, and the antemortem diagnosis remains problematic (1, 2). The cerebrospinal fluid may have evidence of 14-3-3 brain protein, however false positives and negatives may occur (3). Histological analysis of the brain tissue provides the definite diagnosis. The histopathological findings of sCJD are characterized by astrocytosis and neuron loss, being particularly prominent in the putamen and head of caudate nucleus associated with cytoplasmatic vacuole accumulation (4).
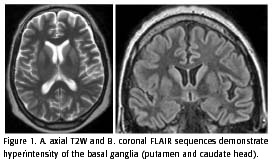
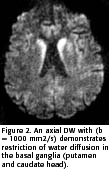
Recently, many authors reported cases of sCJD with typical findings at magnetic resonance imaging (MRI) in 67 to 79% of cases. The patients studied showed classic hyperintensity of the cerebral cortex and basal ganglia (putamen and caudate head) on T2-weighted images (T2W), FLAIR and diffusion-weighted (DWI) sequences, in both the early and late stages (more than 4 months after the onset of symptoms). This finding is indicative of restricted water diffusion and is seen mainly in the basal ganglia. The T1-weighted sequences are usually normal but may demonstrate slight hypointensity in the basal ganglia. The contrast enhancement does not occur (2, 4-10). According to these authors, these typical imaging findings, mainly the DWI findings, in conjunction with the classical clinical presentation, could facilitate the antemortem diagnosis of this rare entity.
We report radiological aspects, structural and diffusion MRI, of two cases with sCJD typical clinical presentation. In the second case, we show the MRI evolution a year and ten months after the onset of the symptoms.
Case 1
Basic biochemical and serological exams were performed and were negative, including HIV and VDRL.
The patient was lost to follow up in October 2001.
Case 2
The patient was a 61 year old man who presented in March of 2001 with apathy, dysarthria and ataxic gait. Rapidly
progressive memory impairment was noticed by family members. The neurological examination, performed two months after the onset
of symptoms revealed sporadic myoclonic facial jerks, dysarthria, quadraparesis associated with extrapyramidal rigidity,
global hypereflexia, bilateral Babinski sign and cognitive impairment.