|
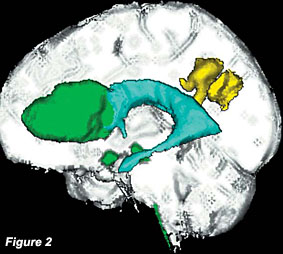
Reconstructed sagittal image of a 3D MR acquisition. Green
represents GBM foci; yellow represents lower grade glioma;
aqua blue represents ventricles |
|
In consideration of
the morphology and of the location of the enhancing lesion the diagnosis of
the glioblastoma multiforme was placed. The patient was sent for a
stereotactic needle biopsy of the frontal mass which conclude for
astrocytoma grade IV (GBM). (Fig2)
The histology
revealed a tumoral proliferation composed of gemistocytes and elongated
cells with fibrillary process. Marked nuclear pleomorphism mitotic figures
and numerous apoptotic cells were also seen as well with an area of necrosis
and foci of endothelial proliferation.
The
immunoistochemistry for GFAP was strongly positive and the proliferation
index estimated by MIB-1 was high, reaching at 15% in a large part of the
tumour. Immunoistochemistry for P53 was also positive. The patient was then
referred for chemotherapy and radiotherapy. |
|
DISCUSSION
Multiple cerebral lesions as the case the Authors described, could represent
GBMs, metastases, even if the primary site of malignancy could not be
identified; lymphoma because of multifocal pattern of lesion with spread
along the corpus callosum, involvement of the infundibulum and the
hypothalamus. However, multifocal GBM, even though the hypothalamus is a
rare location, could result in this pattern and the cortical abnormality in
the left parietal lobe could be compatible with a different stage of the
same pathology and could be considered a low grade glioma.
Multiple high-grade
gliomas (GBM) have been classified as: A) multicentric if they arise
independently in more than one side of the cerebral hemisphere and B)
multifocal if they spread from a primary focus to other areas of the brain.
However this distinction does not have practical clinical value and gliomas
have been categorized as early if they present at the initial diagnosis or
late if they present during the treatment2,3,5. Dissemination can
occur intracranially or throughout the spinal axis and various patterns of
spread have been described in the literature3,4. In the most
recent literature three subtypes of intracranial dissemination based on MRI
characteristic have been described; Type I; a single location of GBM is
present associated to subependymal or subarachnoid spread at sites distant
from the primary tumour location; Type II; a multifocal GBM is present
associated to subependymal or subarachnoid spread; Type III, multifocal GBM
displays subependymal or subarachnoid spread at sites distant from the
primary tumour location.1 According to this classification the
case we describe represents a Type III. To our knowledge no Type III has
been yet described in the literature. In particular the characteristics of
lesions in different degrees of malignancy as suspected on the MRI is an
extremely rare event.
CONCLUSION |
|
In conclusion,
multifocal GBM can be diagnosed on the first MRI as we have illustrated in
this case.
Because of the subependymal spread, we include this unique case as Type III
according to the recent classification proposed by Parsa et al. A focus of
lower grade was likely preexisting in this case, making it a different
subtype. |
|
REFERENCES |
|
1. Parsa AT, Wachhorst S, Lamborn KR et al. Prognostic
significance of intracranial dissemination of glioblastoma multiforme in
adults. J Neurosurg 102: 622-628; 2005
2. Kyritsis AP, Levin VA, Yung WKA et al. Imaging pattern of multifocal
gliomas. European Journal of Radiology 16:163-170; 1993
|
3. Arita N, Taneda M, Hayakawa T. Leptomeningeal
dissemination of malignant gliomas. Incidence, diangosis and outcome.
Acta Neurochir 126: 84-92; 1994
4. Brew BJ, Garrick R: Gliomas presenting outside the central nervous
system. Clin Exp Neurol 23: 111-117; 1987
5. Giese A, Westphal M. Glioma invasion in the central nervous system.
Neurosurgery 39: 235-259; 1996
|
|