|
Cerebral Amyloid Angiopathy Related
Hemorrhage Masquerading as SAH
|
Drs Kevin Petrecca,
Grant
Linnel,
Marie-Christine
Guiot,
John
Richardson &
Denis
Melançon
CASE REPORT |
|
 e
present the case of a 77 year old man who presented with acute paresis of
the left lower face and arm. The patient was otherwise neurologically
intact. One week prior to admission he sustained a fall from his own
height striking his occiput. e
present the case of a 77 year old man who presented with acute paresis of
the left lower face and arm. The patient was otherwise neurologically
intact. One week prior to admission he sustained a fall from his own
height striking his occiput.
A plain CT revealed acute blood in the right central sulcus and inferior
frontal sulcus (Fig. 1A). The presumptive diagnosis was vasospasm
secondary to a traumatic subarachnoid hemorrhage (SAH). A diagnostic
cerebral angiogram, performed to exclude an underlying vascular
abnormality, was normal. The patient was started on Nimodipine resulting
in a significant improvement in symptoms. One week later he developed more
widespread symptoms including right arm weakness. A second plain CT
revealed more extensive hemorrhage with acute blood in the right superior
frontal sulcus, right precentral sulcus and left central sulcus (Fig. 1B). |
|
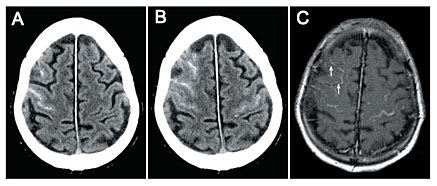
Figure 1. A, CT plain. B,
CT plain. C, T1-weighted MR. Arrows indicate hyperintense signals
restricted to the cortex.
The systemic work-up of a vasculitis was negative. A T1-weighted MRI (Fig.
1C) showed hyperintense signals corresponding to the CT images; however,
the hyperintense signals appeared, in certain regions, to be cortical and
not extracortical (Fig. 1C, arrows). An open left frontal biopsy was
performed for diagnosis. The pathology revealed -amyloid deposition in
blood vessel walls consistent with cerebral amyloid angiopathy. |
|
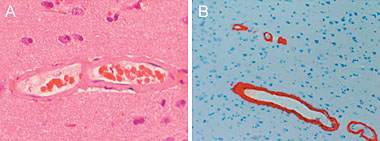
Figure 2. A, H&E stain showing a thickened vessel wall. B,
Blood vessel immunolabelled with an anti-β-amyloid antibody revealing
abundant β-amyloid deposition in the vessel wall.
DISCUSSION |
|
Cerebral amyloid angiopathy (CAA) is a common cause of primary spontaneous
intracerebral hemorrhage. The pathogenesis of CAA involves
b-amyloid
deposition in the media and adventitia of cortical and leptomeningeal
arteries, arterioles, capillaries and less often veins (1). As a result,
vessels become more brittle and thus more susceptible to minor trauma and
changes in blood pressure. As such, CAA-related hematomas are of cortical/subcortical
origin; however, they are not restricted to these regions as they
typically extend deeply into white matter. Here we present an unusual case
of a CAA-related hemorrhage that is strictly confined to the cortex
mimicking subarachnoid hemorrhage on plain CT. |
|
REFERENCE |
|
Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H,
Hanley DF. New England Journal of Medicine. 2001;344:1450. |
|