|
be either enhancing
or non-enhancing. Less frequently, there can be a necrotic mass with a
central non-enhancing zone or a predominantly solid mass with minimal or no
cyst-like component. The precise cause for the often-noted enhancement of
the cyst wall is not well understood and does not seem to correlate with
aggressiveness of the lesion or prognosis.
Macroscopically, as would be anticipated
from the imaging features described above, these tumors are typically
well-circumscribed cyst-like masses with a discrete mural nodule.
Histologically, these lesions demonstrate a ‘biphasic pattern’. Rosenthal
fibers as well as microcysts are often present. It should also be noted that
the relative contribution of the loose and compact tissue components is
highly variable within different tumors. While macroscopically well
circumscribed, there may in fact be microscopic invasion into surrounding
brain parenchyma, but this has not been shown to affect long-term prognosis.
Therapy and Prognosis
Surgical management is the treatment of choice for pilocytic astrocytomas.
Total resection |
|
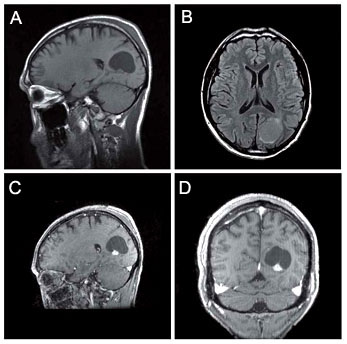
Figure 3: A,
Sagittal T1 pre-contrast.
B, FLAIR image demonstrates that contents of cyst are hyperintense to
CSF. C, Sagittal T1-post gadolinium injection demonstrates
homogeneous enhancement of the mural nodule. D, CoronalT1-post
gadolinium. |
|
Figure 4: A, Loose
microcystic pattern B, Dense fibrillary background C,
Rosenthal fibers References
(1) Bell D et al, “Pilocytic astrocytoma of the adult-clinical
features, radiological features and management.” Br J Neurosurg. 2004
Dec;18(6):613-6.
(2) Burkhard C et al, “A population-based study of the incidence
and survival rates in patients with pilocytic astrocytoma”, J Neurosurg.
2003 Jun;98(6):1170-4.
(3) Koeller KK & Rushing EJ, From the Archives of the AFIP: Pilocytic
Astrocytoma: “Radiologic-Pathologic Correlation” RadioGraphics 2004;
24: 1693-1708. |